When you get out of bed in the morning, do the first few steps make you wince from heel pain? Early-morning heel pain is a classic symptom of plantar fasciitis—inflammation of a band of tissue in the foot called the plantar fascia. At Summit Orthopedics, our foot and ankle care specialists help patients throughout the Minneapolis/St. Paul area move past plantar fasciitis pain. Together, we can find a solution so you can get back to your active life.
What Is the Plantar Fascia?
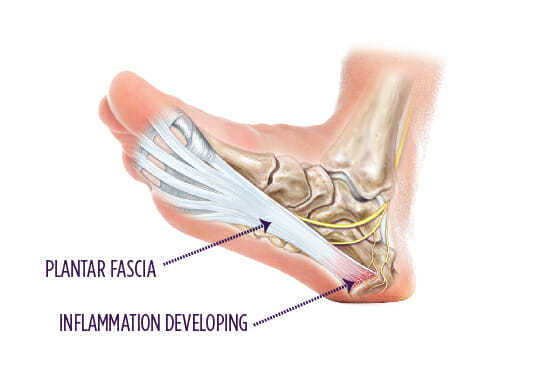
Each step you take puts pressure on your foot, and the plantar fascia ligament is designed to take it. The ligament runs along the bottom of your foot and supports your arch. Even this tough tissue, however, has its limits.
Over time, too much stress can cause tiny tears in the plantar fascia tissue, and it may become inflamed. This inflammation is plantar fasciitis. Left untreated, plantar fasciitis can cause increasing pain and stiffness and make walking difficult.
Risk Factors for Plantar Fasciitis
As you age, your risk for plantar fasciitis rises because of how the ligament changes. Over time, the plantar fascia loses tension, and the shock-absorbing fat in your heel decreases. Both can make the ligament more prone to irritation.
Other factors can put you at risk for plantar fasciitis, including:
- Excess body weight
- Extended time standing on hard surfaces at home or work
- Flat feet
- High arches
- High-impact activities that stress your feet, such as running or dancing
- Starting a new activity or ramping up your activity level too quickly
- Tight calf muscles
Symptoms of Plantar Fasciitis
When inflammation of the plantar fascia occurs, it usually affects the ligament where it attaches to the heel bone. While you sleep, the ligament relaxes. As a result, when you take your first steps in the morning, putting weight on the relaxed ligament, the inflamed tissue may cause heel pain as it stretches. Continuing to move around can help the pain fade.
Be alert for other symptoms of an irritated plantar fascia, including:
- Discomfort when putting pressure on your heel
- Pain after a prolonged period of inactivity, such as riding in a car on a road trip
- Pain after exercising
- Tenderness in the arch
Diagnosing the Problem
If foot pain is interfering with your daily activities, tell your primary care provider, who may send you to a foot and ankle specialist. The specialist will perform a physical exam and check your foot for signs of plantar fasciitis, such as tenderness near the heel and limited range of motion. You may need an X-ray so the physician can check for arthritis, heel spurs and other conditions that can cause heel pain.
Treatments We Offer
Most people with plantar fasciitis find relief using nonsurgical treatments, but be patient—you may need up to 10 months to see improvement.
At Summit Orthopedics, your foot and ankle specialist may start by advising you to take a break from activities that put stress on the plantar fascia and make your symptoms worse. If, for example, running triggers pain, avoid the activity and try one that’s easier on your feet, such as swimming.
In addition to taking time off from high-impact activities, the specialist may recommend other forms of treatment, including:
- Casting to relieve stress on the plantar fascia and give inflammation time to clear up
- Ice to help calm inflammation in the bottom of your foot
- Night splints to stretch the plantar fascia while you sleep and prevent tightening
- Nonsteroidal anti-inflammatory drugs to manage pain and inflammation
- Physical therapy to learn exercises to stretch the plantar fascia and strengthen surrounding muscles
- Regular stretching of your calf muscles, Achilles tendon and plantar fascia
- Supportive shoes and orthotic inserts to provide arch support and cushion your heel
If you don’t see improvement after months of conservative treatment, your foot and ankle specialist may talk to you about whether surgery would be appropriate for you. Most people, however, don’t need surgery for plantar fasciitis.
How to Prevent Plantar Fasciitis
Preventing plantar fascia inflammation isn’t always possible, but you may be able to reduce your risk. Steps you can take include:
- Keep up a stretching program to help your plantar fascia and nearby muscles and tendons stay flexible.
- Maintain a healthy weight.
- Take breaks from standing on hard surfaces.
- Vary your physical activities to avoid putting too much stress on your plantar fascia through overuse.
