Is Total Shoulder Replacement Right for Me?
You may be a candidate for a total shoulder replacement if other treatments for shoulder osteoarthritis have failed to relieve your symptoms. You may be a candidate if you have tried the following treatments without success:
- Physical therapy
- Activity modification
- Anti-inflammatory medication
- Cortisone injections
Additionally, if your pain is negatively affecting your daily activities and keeping you awake at night, you may also be a candidate for total shoulder replacement surgery.
About the Total Shoulder Replacement
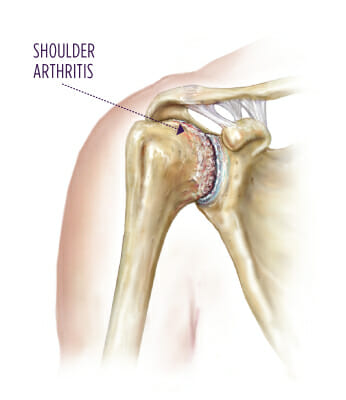
During a shoulder replacement the old, damaged bone and cartilage are removed and replaced with metal and plastic components. All of this work is performed through a four- to five-inch incision on the front of the shoulder.
The joint surfaces that are replaced include the:
- Humeral head (the ball)
- Glenoid (the socket)
There are several different types of shoulder replacements. Your orthopedic specialist will discuss with you the type that he or she feels will yield the best outcome. Typically, both the humerus and glenoid are replaced. There are also instances where only the humeral head is replaced. This decision is usually made during surgery and is based upon the quality of the cartilage surrounding the glenoid.

Preparing for Total Shoulder Replacement Surgery
Several steps need to be completed in the weeks before surgery:
- You must have a preoperative (pre-op) history and physical with your primary care provider within 30 days of surgery. The results should be faxed to the facility where your surgery is scheduled, and you should bring a physical copy of the original form with you to surgery.
- The hospital or surgery center at which you’re having your surgery will typically have a joint replacement education class that you’ll need to attend. You will learn about what to expect before, during, and after surgery. If you choose to have your procedure at one of Summit’s surgery centers, you will benefit from one-on-one joint replacement education with personalized information in an intimate setting.
- Discontinue the use of vitamin E three weeks before surgery.
- Prepare your house for your return after surgery. Simple things like cleaning up any clutter on the floor, clearing space to maneuver a walker, and placing a chair in your shower stall can all help decrease the risk of an accidental fall.
- Any dental procedures need to be completed at least one month in advance of your surgery. In dental procedures, bacteria can enter the bloodstream, causing infection and dramatically affecting your chances for a successful surgical outcome.
- Notify your specialist if you become ill with a cold, fever, congestion, etc., the week before surgery. We may need to reschedule your surgery.
The following will need to be done in the days before surgery:
- Do not drink alcohol for 24 hours prior to surgery.
- Do not take any acetaminophen (Tylenol), ibuprofen (Advil), or other pain medications after midnight the night before your surgery.
- If you are taking prescription blood thinners such as Coumadin (warfarin), Ticlid (ticlopidine), or Plavix (clopidogrel bisulfate), among others, please inform your specialist’s patient care coordinator. These medications will need to be stopped before the procedure, but only after you receive permission from the physician who is prescribing these medications.
- A nurse from the hospital or surgery center will contact you 24 hours prior to surgery to tell you at what time your surgery is scheduled and to answer any questions you may have.

Award-winning shoulder surgical care
Summit Orthopedics has been recognized by the Joint Commission as Disease Specific Certified in Arthroplasty (Shoulder Joint Replacement). Summit Orthopedics is the first freestanding ambulatory surgery center in the U.S. to have the designation. Only four other organizations carry this certification, but none are freestanding ASCs.
The Day of Your Total Shoulder Replacement Surgery
Arrive at the hospital or surgery center two hours prior to your surgery. During this time, your nurses may run minor tests, check your blood pressure, and take your pulse. Your anesthesiologist will meet with you to discuss the type of anesthesia you will receive.
For more information, please refer to the presurgery handout you received.
Antibiotics are administered prior to surgery to help protect against any potential infection. During this time, your family may remain with you until you are taken to surgery. A member of your specialist’s team will also come in and address any last-minute questions or concerns you might have.
What Can I Expect After Total Shoulder Replacement Surgery?
Total shoulder replacement surgeries can be performed either at a hospital or at the Vadnais Heights Surgery Center or Eagan Surgery Center.
- Initially, you will be placed in a recovery room for several hours so that we can monitor you closely as the anesthesia wears off. During this time, your family will be notified that the surgery is complete and that you are in recovery.
- After the effects of the anesthesia have worn off and you are medically stable, you will be moved to a hospital or Care Suites room, and your family will be able to visit you.
- Most joint replacement patients go home the same day if they have their procedures done at a surgery center. Some patients choose to stay in the Care Suites overnight. If a patient chooses to have the surgery in the hospital, the patient is generally admitted for one or two nights.
- During your stay, you will participate in physical therapy several times a day.
Contact your specialist immediately if you develop a fever or chills, have pain that is not relieved by medication, have excessive unrelenting drainage or calf pain, or if you fall. Call 911 immediately if you experience any shortness of breath or develop chest pain.
What to Expect For Leaving the Hospital or Care Suites
Before surgery, you and your physician will establish a plan for where you will be discharged after surgery and who will be caring for you. After you go home, you’ll come to our physical therapy facility twice a week for ongoing rehabilitation.
What to Expect For Your First Follow‑Up Visit
After surgery, your treatment team will want to see you in clinic. At this appointment, you can expect to have any remaining staples removed, have X-rays taken, and receive instructions and guidelines for the next four to six weeks. Your specialist will provide you with physical therapy orders and can write a referral to a physical therapy clinic if you need it.
Potential Complications During and After Total Shoulder Replacement Surgery
It is important to have realistic expectations about your total shoulder replacement surgery. Although they are rare, there are potential complications with any surgery, and you are expected to have a reasonable understanding of the risks. Please refer to our preoperative informational handout for further information regarding potential complications and risks associated with surgery.
Our goal at Summit Orthopedics is to assist you in this regard and help you have the best experience possible as you transition into this new phase of your life. Should you have any questions or concerns, please contact your specialist’s team. They are available to help you and address any questions or concerns that you may have.
Considering Shoulder Replacement?
If shoulder pain is affecting your daily life, our team is here to help. Summit Orthopedics offers expert evaluation and personalized treatment options at convenient Twin Cities and Western Wisconsin locations.
