What is knee arthritis?
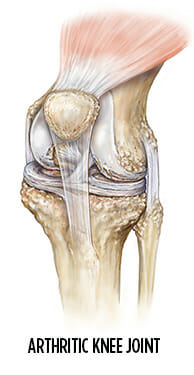
Before we can understand knee arthritis, it’s important to know that the knee joint is composed of three bones:
- The femur (thighbone)
- The tibia (shinbone)
- The patella (kneecap)
In a healthy knee, flexible connective tissue called cartilage coats the end of these bones and a thick liquid lubricates it. This allows for smooth, normal movement.
When a knee joint develops osteoarthritis, it means that the cartilage has worn away and the joint surface has become rough and irregular. This prevents the joint from moving correctly. As the cartilage wears down, the knee bones rub against each other. This results in further damage, increased pain, and bone spurs.
What causes knee arthritis?
Age is the most common cause of knee osteoarthritis, since the ability of cartilage to heal decreases as we get older. Most people will eventually develop some degree of arthritis.
The following factors increase the risk of developing significant arthritis at an earlier age:
- Excessive weight — being overweight or obese increases pressure on all the joints, especially the knees
- Genetics — some people are more likely to develop arthritis based on the shape of their bones around the knee
- Gender — women who are 55 and older are more likely than men to develop arthritis of the knee
- Repetitive stress injuries — people with jobs requiring a lot of kneeling, squatting, or lifting of heavy weights are at increased risk for knee arthritis
- Other illnesses — people with rheumatoid arthritis are more likely to develop osteoarthritis. Other metabolic disorders also increase the risk of osteoarthritis.
What are the symptoms of knee arthritis?
Symptoms of knee arthritis typically develop gradually and include:
- Pain and swelling
- Clicking or grinding sensation
- Decreased ability to move the joint
- Difficulty standing or walking for extended periods of time
- Difficulty sitting for extended periods of time
- Difficulty getting out of a chair
How is knee arthritis diagnosed?
Your doctor will diagnose knee arthritis based on:
- Your medical history
- Your symptoms (such as the location of the pain)
- The activities that make the pain better or worse
- A physical examination of the movements and strength of your knee
If knee arthritis is suspected, an X-ray will typically confirm or deny the diagnosis.
How is knee arthritis treated nonsurgically?
The severity of your arthritis will determine the most appropriate course of action. For early-stage arthritis, effective treatments include:
- Physical therapy
- Anti-inflammatory medication
- Weight loss
Research suggest that certain diets and supplements may be helpful in treating arthritis, including:
- Fish oil
- Turmeric
- Anti-inflammatory diets
In more advanced cases, the following can be effective at relieving your symptoms:
Activity modification
Patients with arthritis typically have to undergo some lifestyle modifications. If specific activities make your symptoms worse, then avoiding those activities can provide relief. Low-impact exercises such as cycling, elliptical, swimming, and light strength training are the best options.
Anti-Inflammatory medication
Oral anti-inflammatory medicines may be effective at decreasing inflammation associated with osteoarthritis. However, some people suffer from side effects while taking them. If you experience anything unusual when taking these medications, contact your doctor immediately to determine if continued use is appropriate.
Unloader knee braces
Your doctor may prescribe an unloader brace. This brace relieves the pressure on the worn area of the joint. You will need to wear this brace when participating in such activities as walking, hiking, and sports. For some, this brace may provide significant symptomatic relief, allowing the enjoyment of physical activity again.
Steroid injections
A steroid injection allows your doctor to place anti-inflammatory medication directly inside the joint. This can result in dramatic and potentially long-term relief of pain and swelling. If this does provide relief, you can safely have repeat injections done every three to four months without any harmful effects.
There is no limit to the total number of knee injections you can have, and long-term steroid injection treatment does not cause any further damage to the joint.
Physical therapy
Your physician may prescribe several sessions with a physical therapist to increase your range of motion and strength, and to decrease your pain. Physical therapy combined with weight loss is as effective in treating osteoarthritis pain as some anti-inflammatory medications.
After several visits, your therapist may recommend a home exercise program to help maintain any gains you have achieved during therapy.
Joint fluid therapy
In this treatment, hyaluronic acid is injected into the knee. It can be done all at once or in three doses, typically spaced one week apart. The injection helps to reduce friction between rough cartilage while cushioning the joint. This treatment can be done every six to nine months if your symptoms warrant it. Further information regarding this medication can be provided to you upon your request.
Ice
Ice is a convenient and inexpensive treatment option for knee pain. Placing a bag of ice directly on the knee for 20 minutes prevents swelling and inflammation from occurring inside the knee.
What are the surgical treatment options for knee arthritis?
In the case of severe arthritis, surgery may be the best treatment option.
Knee Arthroscopy
In this surgery, the physician will use a miniature video camera and tools to remove any loose cartilage. The result is a smooth joint surface free of loose tissue and minimal internal derangement that can cause irritation.
Arthroscopy can provide significant relief and allow the joint to flow freely through its range of motion. Arthroscopy can be effective in early arthritis and may be used to treat associated conditions that could lead to more severe osteoarthritis down the road, but is typically not effective in advanced osteoarthritis.
Total knee replacement
In advanced cases of arthritis, you may be a candidate for a total knee replacement. The techniques and prosthetics used in this surgery have made significant advances over the past decade. Patients who undergo a total knee replacement are living longer and getting more use out their new joints than ever before.
Learn more about total knee replacement.
How can I prevent knee arthritis?
There are things you can do to reduce the risk of developing osteoarthritis in your knees. The less stress you put on your joints, the less likely they are to wear out prematurely. Try to:
- Maintain a healthy weight
- Exercise to strengthen muscles around joints
- Use good posture
- Rest if joint pain starts to bother you
- Start new activities slowly and safely until you know how your body will react
When to seek treatment for your arthritis
Arthritis doesn’t have to spell the end of an active life. If you are experiencing worrisome symptoms or persistent pain, the renowned arthritis specialists at Summit Orthopedics can help. We work with you to confirm a diagnosis and develop an appropriate conservative treatment plan. If nonsurgical treatments fail to support your lifestyle goals, fellowship-trained orthopedic surgeons will consult with you and discuss appropriate surgical options. Summit is home to innovative joint replacement options. Our Vadnais Heights Surgery Center is one of a select few nationally to receive The Joint Commission’s Advanced Certification for Total Hip and Total Knee Replacement.
Start your journey to healthier joints. Find your arthritis expert, request an appointment online, or call us at (651) 968–5201 to schedule a consultation.
Summit has convenient locations across the Minneapolis-St. Paul metro area, serving Minnesota and western Wisconsin. We have state-of-the-art centers for comprehensive orthopedic care in Eagan, MN, Vadnais Heights, MN, and Woodbury, MN, as well as additional community clinics throughout the metro and southern Minnesota.
